Dear all Just finished a great 2 day tendinopathy course in Melbourne – lots of great tendinopathy clinical discussions, ie the nitty gritty of treating tendons – what to assess, how to treat! Please contact me to organize a course in your part of the world [email protected] Here is the latest in tendon research. Best wishes Peter Sunsararajan et al. found that patients with insertional Achilles pain have a greater Chauveaux-Liet angle (c) than those without. May relate to compression. Retrospective study so huge limitations, such as patient selection, and imaging assessors were not blind. www.ncbi.nlm.nih.gov/pubmed/24556480
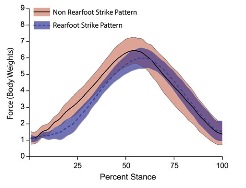
Zhang et al. – Ice on the Achilles and patellar tendon after exhaustive treadmill running in rats reduced levels of PGE2. May have positive influence on reducing tenocyte overstimulation and even pain following load. May not be practical – applied ice for 30 minutes, and may need to be longer for deeper tendons, joints. www.sciencedirect.com/science/article/pii/S2214031X14000163 Sobhani et al. – interesting study showing that rockerbottom shoes reduced the planterflexion moment and impulse, coinciding with a small (3 degree) reduction in ankle DF in late stance. May be a better option than a heel wedge in some groups, e.g. older, restricted sagittal plane ankle/foot http://www.ncbi.nlm.nih.gov/pubmed/24636129 Kosters et al. have shown that patellar tendon stiffness is dependent on loading rate, ie increased stiffness with faster loading rate. Need to factor this in when comparing stiffness between studies and over time. www.ncbi.nlm.nih.gov/pubmed/24405566 Becker et al. have shown late pronation in runners with vs without Achilles pain. Makes a lot of sense that lack of foot function as a lever, or even spring via the plantar fascia, will lead to calf-Achilles overload. http://www.asbweb.org/conferences/2013/abstracts/184.pdf Almonroeder et al. – within subjects design comparing rearfoot and non-rearfoot running (most habituated from natural rearfoot for the study, rather than the other way). No significant difference in peak Achilles force although it occurred earlier for non-rearfoot strike (see figure below). There was a trend (p=0.06) towards greater average loading rate (15% greater) in the non-rearfoot strike group. Stance time was similar between groups. www.ncbi.nlm.nih.gov/pubmed/23640524
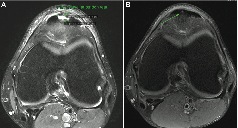
De Vos et al. – systematic review of 6 randomised studies investigating PRP injection in lateral elbow tendinopathy. Three out of four high quality studies show that it is not effective ! authors state…”Popularity of PRP is growing in relation to marketing, positive lab studies, clinical case series, and narrative reviews”. Could not agree more bjsm.bmj.com/content/early/2014/02/21/bjsports-2013-093281.abstract Wearing et al. – lovely study investigating fluid flow out of the Achilles and patellar tendons with loading. Quads were loaded with squats, and calf with calf raises. Tendon thickness immediately reduced 14-18% (fluid flow out of the tendon) in both tendons and took 6-7hrs to recover (see figure below, showing ratio of follow up to initial thickness over time). Link between fluid flow, mechanotransduction and injury is unclear. Maybe loading a water depleted tendon causes injury? Or maybe tendons that don’t have as much fluid flow have altered mechanotransduction and increased risk of injury? www.ncbi.nlm.nih.gov/pubmed/235255544 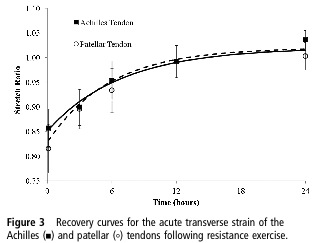 Charousset et al. – case series of 28 patellar tendinopathy patients who had 3 PRP injections over 3 weeks. 21 out of 28 returned to preinjury sport level at 3 months. Needs to be interpreted with huge caution given the study design – we need RCT’s not more case series! What is most surprising is ‘complete return to normal tendon structure on MRI’ in 57% of tendons, assessed by a radiologist blinded to treatment (see example below) – I have never seen this with ultrasound after PRP injection to the patellar tendon – is ultrasound more sensitive? www.ncbi.nlm.nih.gov/pubmed/24519184
Charousset et al. – case series of 28 patellar tendinopathy patients who had 3 PRP injections over 3 weeks. 21 out of 28 returned to preinjury sport level at 3 months. Needs to be interpreted with huge caution given the study design – we need RCT’s not more case series! What is most surprising is ‘complete return to normal tendon structure on MRI’ in 57% of tendons, assessed by a radiologist blinded to treatment (see example below) – I have never seen this with ultrasound after PRP injection to the patellar tendon – is ultrasound more sensitive? www.ncbi.nlm.nih.gov/pubmed/24519184
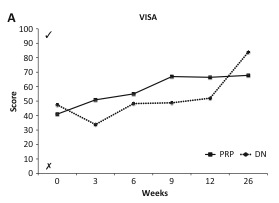
Peterson et al. – compare eccentric vs concentric elbow loading for lateral elbow tendinopathy, using an Alfredson framework, ie 3×15 daily. Both groups improved similarly at 12 months, eccentric group improved faster. More of the concentric group had previously had exercise as a treatment (15% v 5%, p=0.07). Also, why not compare eccentric to concentric-eccentric. Who ever does isolated concentric? cre.sagepub.com/content/early/2014/03/14/0269215514527595.abstract Dragoo et al. – another PRP study I’m afraid. This study compared single dry needling with PRP procedure, both groups performed eccentric loading. The dry needling group was significantly older and had an oddly ‘old’ mean age for patellar tendinopathy (40 +/-14 years compared with 28+/-8 years). VISA improved more in the PRP group initially, but the dry needling group caught up by 26 weeks (see figure – significantly better at 12 weeks, not 26 weeks). Overall modest improvement in the PRP group at 26 weeks – appropriate loading would likely improve on this outcome www.ncbi.nlm.nih.gov/pubmed/24481828
Foster et al. did not find an association between the COL5A1 rs12722 gene variant and Achilles tendon patellar tendon volume. Previously, this genetype phenotype has been associated with risk of tendinopathy, so this relationship is likely mediated by other factors www.ncbi.nlm.nih.gov/pubmed/24643429 Huberts and van Cingel 2013 – systematically reviewed eccentric training protocols in the Achilles, with a focus on the influence of training parameters on outcome. The major conclusion is that not sticking to a stringent Alfredson 3×15 twice daily protocol (for example, building up gradually to 3×15) can still achieve good outcomes. This is even though compliance can be low – 26-72% in the three studies that measured it. Key underlying point is, many people do not respond to this one size fits all protocol – reported to be 24-45% (Alfredson 2000, Longo 2009). http://onlinelibrary.wiley.com/doi/10.1111/sms.12208/abstract;jsessionid=F3E552933570B36B02D26F8947D66802.f02t03?deniedAccessCustomisedMessage=&userIsAuthenticated=false Alfredson H, Lorentzon R. Chronic Achilles tendinosis: recommendations for treatment and prevention. Sports Med 2000: 29: 135–146. Longo U, Ronga M, Maffulli N. Achilles tendinopathy. Sports Med Arthrosc Rev 2009: 17: 112–126. Joseph et al. – great study investigating Achilles tendon properties after light (10 minute treadmill walk) and heavy exercise protocols (100 toe jumps in a Smith machine with +20% of their bodyweight). Young’s modulus decreased significantly after the jumping protocol but only among women, not men. May tie in with recent fluid flow research from Wearing, Grigg, ie increased compliance likely related to fluid flow out of the tendon. So having less fluid flow may be detrimental, negatively affecting mechanotransduction? www.ncbi.nlm.nih.gov/pubmed/24552794 Pingel et al. 2014 – took biopsies from 6 tendinopathy patients, and from normal tissue around the tendinopathy. Tendinopathy areas showed increased type III compared with type I collagen, and bucking of the ECM and tenocytes seen with electron microscope. http://onlinelibrary.wiley.com/doi/10.1111/joa.12164/abstract Visnes et al. – prospective study of patellar and quads tendon US and pain changes over 1-4 years (average 1.7 years) among elite junior volleyball players. Patellar tendon thickness increased in those that developed symptoms. Presence of hypoechoic region (OR=3.3) or neovascularization (OR=2.7) increased the risk of developing patellar tendinopathy symptoms. Interestingly, 17% of tendons were normal on US at time of symptom onset, and only 17/46 (36%) of tendons with hypoechoic areas at baseline developed symptoms. This study highlights that structural US changes do not equal symptoms, and although they predict future symptoms, many with structural changes do not develop pain even though they are loading heavily. http://www.klokavskade.no/upload/Publication/Visnes_2014_SJMSS_Ultrasound%20characteristics%20of%20the%20patellar%20and%20quadriceps%20tendons%20among%20young%20elite%20athletes.pdf