Hip pain is not a condition reserved for the elderly.
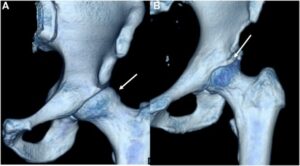
More and more hip pain research is being directed at understanding the cause and burden of hip pain on patients aged 18-50. One such condition being investigated is femoroacetabular impingement (FAI) syndrome, a condition characterised by changes to the bone formation in the neck of the femur (thigh bone) and acetabulum (hip joint socket). In younger athletes, hip pain symptoms may occur as a result of the hip joint movements and forces associated with sporting demands, and is common in agility and kicking sports such as football1. In my clinical experience, some patients with mild hip joint symptoms may present complaining of persistent “hip flexor tightness”, and this misdiagnosis can delay appropriate treatment.

When confronted with a hip pain patient, a thorough assessment helps guide the patient’s exercise program. Patients with FAI syndrome consistently demonstrate strength deficits3, and report pain at the extremes of joint movement. When designing an exercise program for a patient, we must ask:
How do you know if something needs to be strengthened, if you don’t know if it is weak?
And just as importantly for busy patients (who are sick of doing exercises!), why do an exercise if you don’t need to do it?!?
Clinically, I find hand held dynamometry (HHD) to be a valuable tool to identify these weaknesses, and also monitor the effect of exercise programs. HHD uses a small device to measure the amount of force produced when we do a strength test, and it has been shown to be a reliable measure2.
Exercise for hip pain, what’s news?
Some important research by Kemp et al (2018)4 highlights that physiotherapy-led exercises have been shown to improve pain, function and quality of life in patients with hip pain. (The paper can be found here: https://www.ncbi.nlm.nih.gov/pubmed/29607766)
In this pilot study, participants were treated by a physiotherapist with a combination of manual therapy, supervised exercise and a home exercise program. The exercise program specifically targeted the deficits seen in patients with FAI syndrome and was completed over a 3-month period. This exercise program produced VERY LARGE treatment effect sizes, greater than surgical and other physiotherapy exercise programs seen elsewhere5. A real positive of this study’s design is that the dosage of exercise and the length of the program was appropriate to produce improvements in strength and ROM… i.e. it takes time to make meaningful changes to joint ROM and muscle strength!
Interestingly in this study, improvements in hip flexion ROM, adduction (groin) strength and trunk strength were most associated with improved outcomes. While this is only a small pilot study, we look forward to seeing the results of the large scale trial in the future.
What does this mean for patients with hip pain who currently have symptoms?
- TRY EXERCISE FIRST before considering surgery. Exercise programs should be of at least 3 months duration to allow for adaptation of tissues!
- Measure your strength, ROM and function with a thorough clinical assessment by your physiotherapist.
- Target your exercise program to what you need – don’t strengthen something that is already strong, and don’t mobilise something that is already mobile!
- Correct faulty movement patterns. Address walking, squatting, and/or running technique to maximise efficiency and reduce excessive hip joint loading.
- Apply enough load. If strengthening is your goal, then apply strengthening principles – too little load and you might be wasting your time!

References:
- Werner J, Hägglund M, Waldén M, Ekstrand J. UEFA injury study: a prospective study of hip and groin injuries in professional football over seven consecutive seasons. British Journal of Sports Medicine. 2009;43(13):1036-1040.
- Thorborg, K., Petersen, J., Magnusson, S. P., & Holmich, P. (2010). Clinical assessment of hip strength using a hand-held dynamometer is reliable. Scandinavian Journal of Medicine and Scince in Sports, 20: 493-501.
- Freke, M. D., Kemp, J., Svege, I., Risberg, M. A., Semciw, A., & Crossley, K. M. (2016). Physical impairments in symptomatic femoroacetabular impingment: a systematic review of the evidence. British Journal of Sports Medicine, 50: 1180-1199.
- Kemp, J. L., Coburn, S., Jones, D., & Crossley, K. M. (2018). The physiotherapy for femoroacetabular impingement rehabilitation study (PhysioFIRST): a pilot randomized controlled trial. Journal of Orthopaedic and Sports Physical Therapy, 48(4): 307-315.
- Griffin, D. R., Dickenson, E.J., Wall, P. D., et al (2018). Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicenter randomized controlled trial. Lancet, 391(2): 2225-35.