When managing patients with hip joint pain, my 5 general rules are:
- Don’t allow imaging findings to become a burden carried for life – they may be irrelevant.
- Perform a thorough clinical examination to identify a symptomatic hip joint and rule out other sources of pain (e.g. lumbar spine referral, tendon injury to the lateral hip). Do we confirm or question the results of the imaging?
- Identify measurable impairments which may be contributing to the persistence of pain (e.g. loss of strength, range of movement, movement control, balance). What are your deficits as a result of the pain?
- Identify contributing factors which may increase the likelihood of hip pain (e.g. weight, training load, work or sporting demands). What other things might be contributing?
- Undertake a structured, targeted rehab program to address these deficits. Make sure to continue to progress your exercise… it needs to be a challenge!
Let’s unpack rule number 1.
Magnetic resonance imaging (MRI) can visualise both bony and soft tissues, and can be very useful in confirming a clinical diagnosis. For example, an MRI can confirm a clinical suspicion of an ACL injury in the knee (e.g. following a twisting injury while playing sport). For injuries that develop slowly (e.g. 2 months of gradual onset hip pain with no incident), the role of MRI is less definitive. In these cases, findings must be interpreted with caution.
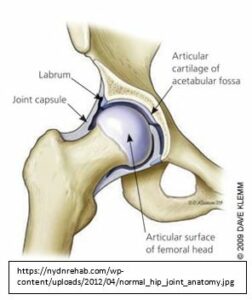
In its simplest form, the hip joint is a ball and socket joint made up of the bony head of the femur and the acetabulum of the pelvis. The rim of the socket is lined with a cartilage labrum which is thought to deepen the socket and contribute to maintaining joint ‘stability’. The joint surfaces are covered with articular cartilage, through which weightbearing forces are transmitted.
Many structures within the hip joint can be ‘injured’ or overloaded and become a source of pain. Often, injuries to multiple structures can occur at the same time, making a specific diagnosis of your hip pain complicated.
So, you have had your hip joint MRI…
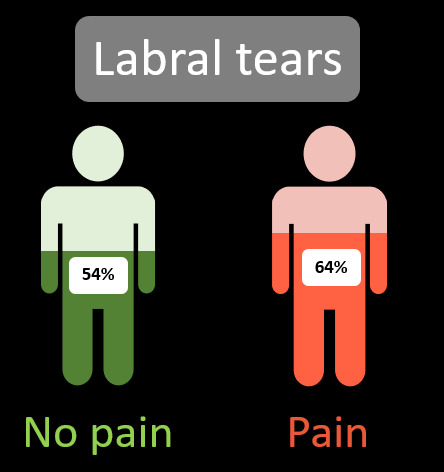
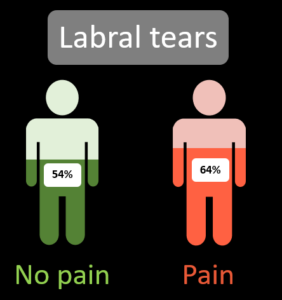
MRI scans will often lead to patients receiving a “diagnosis” of a labral tear. This is an injury to the labrum, the cartilage rim of the socket. Due to its role in deepening the socket, patients can be told that the “stability” of their hip is now compromised following their labral injury. Labral tears are common in people with hip pain, with 62% of people with hip pain having a labral tear on MRI [1].
However, 54% of people without pain also have a labral tear [1]. (yep, 1 in 2 people without pain)
Important questions that we must ask:
- Is it likely that the labrum is the primary source of pain in someone with hip pain?
- Do people with a labral tear and no pain have an “unstable” hip?
- Does this make them more likely to develop pain in the future?
OR,
- Are these findings a normal variation for healthy adults?
Large scale longitudinal studies over many years are needed to answer these questions. But if we take lessons from other joints of the body, a labral tear in isolation may be unrelated to the development of hip pain.
So, what about athletes & hip pain..
Interestingly, if we consider only studies that have investigated athletes with and without hip pain, we see a similar message from the research. A recent systematic review found that:
Athletes without hip pain had a higher prevalence of labral tears than athletes with pain on MRI [2].
In clinical practice we don’t make a habit of imaging people without pain, so we must use these studies to put these imaging “findings” into context. 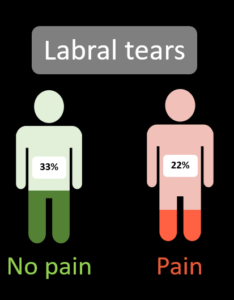
Findings such as a labral tear in patients with hip pain continue to be used as justification for surgical intervention. However, considering the high rates of labral tears in people without pain we must question this rationale.
So, it might not be the labrum, what about other structures within the hip joint?
Imaging findings relating to the articular surface cartilage appear to be more common in people with pain [1].
Similar rates of cartilage findings are seen in athletes too [2], suggesting that the presence of cartilage findings may have a greater role in influencing hip pain.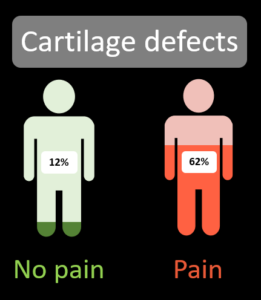
Interestingly, the joint surface cartilage is not thought to be pain producing, so it may be changes in other structures (eg. joint fluid, bone beneath the joint cartilage) which may occur in conjunction with these cartilage findings which may influence pain.
Again, more research is needed to identify the mechanisms of hip joint pain.
An important take home message from previous research summarised by the 2 systematic reviews discussed in this blog is that while joint surface cartilage findings are more common in people with pain, the relationship between labral findings and pain is less clear. Clinical decision making for patients with hip pain should not be based solely on the presence of imaging findings of “pathology”.
I will discuss rules 2-5 in later blogs
References:
[1] Heerey, J.J., et al. (2018). What is the prevalence of imaging-defined intra-articular hip pathologies in people with and without pain? A systematic review and meta-analysis. British Journal of Sports Medicine, 52(9): p. 581-593.
[2] Heerey, J. J. et al (2019). What is the prevalence of hip intra-articular pathologies and osteoarthritis in active athletes with hip and groin pain compared to those without? A systematic review and meta-analysis. Sports Medicine, 49: p. 951-972.