Dear all
Has been a while since the last installment and there have been lots of enthusiastic researchers publishing their excellent work – here is some.
More to follow in a ‘Christmas Special’, back end of December, as there are lots of other great studies over the last 3 months I would like to include.
I hope you enjoy
Peter
Studies that directly change our practice
www.ncbi.nlm.nih.gov/pubmed/25367547
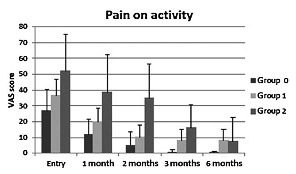
This study takes centre stage as it focuses on an exercise intervention for Achilles tendinopathy – about time someone did! Wetke et al 2014 report on a pragmatic case series design of a sensible graduated strength/power program for Achilles patients. The rehab included 3×20 double then single leg calf raises on flat ground, progressing to a 2cm then 5cm book – they progressed when the exercise was no longer causing pain aggravation. Then they progress to jump/walk/run but how is not fully elucidated. They offered steroid injections to people who had pain limiting rehab and crepitus on imaging signs of bursitis or paratedinitis. Patients were offered injections (if indicated) at each of the 4 follow up visits, baseline, 1, 2, 3 months, during the 3 month intervention period. All injections were deep to the tendons, between the tendons and adjoining Kager’s fat. 93 patients completed the study, 43 women, 40 men, 73% active in sports. Twenty four percent had only rehab, 58% rehab+1 injection, 14% rehab+2 injections, 2% rehab+3 injections. The primary end point was 6 months and primary outcomes were global improvement and pain with 20 one leg calf raises, and secondary outcomes were morning pain, duration of morning stiffness, and max US thickness.
Pain with one leg calf raises improved significantly at each time point – see figure below. 78% had an excellent or good outcome. However, only 58% of sports active participants were back 76%-100% of their prior sports activity at 6 month follow up. Insertional patients showed only a tendency for improvement in pain with activity, otherwise they improved on all outcomes like the midportion group.
Steroid lead to improvements in all outcomes, as expected, in the short term. There was no ‘recurrence’ aside from significant worsening but still better than baseline result for morning pain at final outcome (mean 4.9 months, a some had the injections after baseline). As expected as well, rehab was a slow burner, all outcomes were improved at final 6 month but not shorter follow ups.
This study supports prior research that exercise has a slow and lasting effect, steroid has an amazing but short lived effect and may be detrimental in the longer term. Regardless, using steroid as an adjunct to allow Achilles rehab is certainly not completely rejected by these data, in contrast to the Coombes et al. 2013 study – the difference in this study was that exercise+adjuncts alone did not produce any positive effects and steroid injections were intra- as apposed to extra-tendinous in this study.
Coombes BK, Bisset L, Brooks P, Khan A, Vicenzino B. Effect of Corticosteroid Injection, Physiotherapy, or Both on Clinical Outcomes in Patients With Unilateral Lateral EpicondylalgiaA Randomized Controlled TrialCorticosteroid & Physiotherapy for Epicondylalgia. JAMA. 2013;309:461-469.
www.sciencedirect.com/science/article/pii/S0966636214007279
Franz 2014 used motion capture, ultrasound and treadmill force plate data to estimate change in length of different regions of the Achilles tendon during walking. The key finding is that there was 16-29% greater elongation in the superficial compared with deep AT during the stance phase of walking-see figure below. Supports the stress shielding hypothesis (e.g Almekinders et al. 2003), i.e. reduced stress in the deep portion of the tendon. They also showed that peak elongation increased significantly with walking speed, but only in the superficial not deep AT – this increase elongation with speed was matched by similar increase in soleus and gastroc EMG activity. It has been reported from one anatomical study that superficial fascicles arise from the medial gastrocnemius and deeper fascicles arise from the and lateral gastrocnemius (Szabo et al. 2009) (albeit on limited evidence), so non-uniform elongations may influence different parts of the calf muscle.
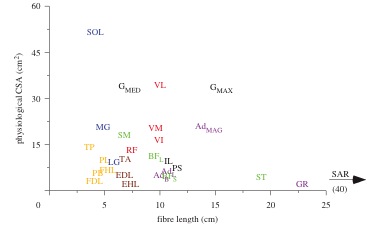
I suspect this finding is related to increased DF range at faster speeds (which is reported in the study) and the moment arm differences between the deep and superficlal Achilles tendon. This fits with prior research that there are different strain gradients with active and importantly passive movements (Slane 2014), so may not be driven my muscle activity. May lead to secondary issues, eg increased soleus elongation – remembering that soleus has a relatively short fascicle length (see figure below from Lieber and Ward 2011, SOL = soleus) this may compromise length tension and is a good reason to consider end range load for Achilles patients when there are no reasons not to.
Szaro P, Witkowski G, Smigielski R, Krajewski P, Ciszek B. Fascicles of the adult human Achilles tendon – an anatomical study. Ann Anat 2009;191:586-93.
Almekinders LC, Weinhold PS, Maffulli N. Compression etiology in tendinopathy. Clin.Sports Med. 2003;22:703-710.
Szaro P, Witkowski G, ?migielski R, Krajewski P, Ciszek B. Fascicles of the adult human Achilles tendon–an anatomical study. Annals of Anatomy-Anatomischer Anzeiger. 2009;191:586-593.
Slane LC, Thelen DG. Non-uniform displacements within the Achilles tendon observed during passive and eccentric loading. Journal of biomechanics. 2014;47:2831-2835.
www.ncbi.nlm.nih.gov/pubmed/25243736
Interesting study by Mike Reiman et al. – they review studies that investigate sensitivity (screening, ie ruling out) and specificity (diagnosis, ruling in) of tests in Achilles rupture (1 study) and Achilles tendinopathy (2 studies). The classic calf squeeze test came out on top for diagnosing Achilles rupture. The sensitivity and specificity of diagnosing rupture was generally greater than tendinopathy. Crepitus, the arc sign, the Royal London Hospital test, single-legged heel raise, and tendon thickening demonstrated strong specificity – these can help to confirm a diagnosis of Achilles tendinopathy. Only morning stiffness and palpation demonstrated moderate sensitivity – if these are absent it goes some way towards ruling out Achilles tendinopathy.
The main issue with this literature is that they always compare diagnostic tests to pathology – so they tell us if the tests help to rule in or out pathology, which is sometimes but not always related to pain. What would be great is tests that could differentiate some of the tricky Achilles differentials eg plantaris vs Achilles midportion vs acute paratenon. My clinical experience is that tests like the London Hospital test help to differentiate midportion pain from some of these differentials. To test this we need to look at typical symptoms+imaging confirmation for these differentials, eg plantaris would be medial localized pain, pain in end range dorsiflexion and US confirmation of plantaris pathology. Obvious difficulties with this approach would be finding enough cases that fit these specific diagnostic criteria.
Other interesting studies
www.ncbi.nlm.nih.gov/pubmed/25037955
Crill et al. investigated change in fascicle length, pennation angle and muscle thickness following 6 weeks of eccentric training in Achilles tendinopathy patients. Only medial gastrocnemius fascicle length increased during the study. The authors suggest (but did not measure) that there would have been an associated rightward shift in the length tension curve, and that greater force producing potential in more extreme ranges may be a mechanism of action of eccentric training. The main issue is they did not measure soleus which and there is evidence emerging thanks to Seth O’Neill as ISTS 2014 (reported in previous blog post) that this may be selectively weak in Achilles patients.
www.ncbi.nlm.nih.gov/pubmed/25277276
Interesting study by Kubo et al. found no relationship between habitual forefoot, midfoot and reafoot striking and Achilles stiffness in elite endurance runners. However, the sample was relatively small (12 forefoot, 12 midfoot, 17 reafoot strike), and it is possible that given they were all elite, they were homogenous, ie had relatively stiff tendons. It may be that a novice runner who transitions to forefoot running may develop a stiffer Achilles over months, as has been suggested by Blais Dubois and makes sense, but they also run the risk of foot and ankle injury as we know.
www.ncbi.nlm.nih.gov/pubmed/25158908
Moulton 2014 et al. have found that acetabular anteversion measured on MRI is associated with an MRI diagnosis of gluteal tendinopathy. Femoral neck angle was not associated, in contrast to the study by Angie Fearon. In the Fearon et al. 2012 study they had a smaller sample and femoral neck angle was associated with only those going onto have gluteal reconstructive surgery.
Fearon A, Stephens S, Cook J, et al. The relationship of femoral neck shaft angle and adiposity to greater trochanteric pain syndrome in women. A case control morphology and anthropometric study. British Journal of Sports Medicine. 2012;46:888-892.
http://www.readcube.com/articles/10.1371%2Fjournal.pone.0108337
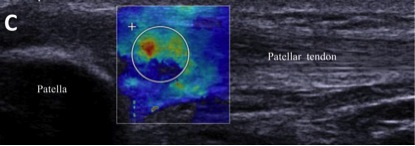
Zhang et al. measure shear wave elastography in patellar tendinopathy. This is a relatively new imaging modality that is different to compression elastography that is currently being used clinically – the difference is it is not operator dependent AND it gives a measure of tensile stiffness just from an ultrasound image – amazing! The authors compared tendon stiffness in the pathological region of interest on the painful and non painful sides of people with unilateral patellar tendinopathy. They found increased stiffness on the painful and more pathological side. Contrasts previous findings of reduced stiffness in pathological Achilles and patellar tendons (Helland et al. 2013, Arya et al. 2010). Most likely due to location of region of interest and technique, previous studies measure with ultrasound in vivo during MVC, Zhang measure with this whiz bang new elastography technique, focusing on the pathological area (see image below). The total tendon response may be a compensation for a focal increase in stiffness at the pathology site, ie perhaps allows an equivalent amount of strain in functional energy storage activities (eg jumping, running). I predict shear elastography will be the next big thing in tendon clinical imaging, overtaking UTC, which still lacks adequate human validation. Shear wave could identify early changes in stiffness and guide rehab – much more research needed.
Helland C, Bojsen-Møller J, Raastad T, et al.: Mechanical properties of the patellar tendon in elite volleyball players with and without patellar tendinopathy. British Journal of Sports Medicine. 2013, 47:862-868.
Arya S, Kulig K: Tendinopathy alters mechanical and material properties of the Achilles tendon. J Appl Physiol. 2010, 108:670-675.
www.ncbi.nlm.nih.gov/pubmed/25056989
Huttunen et al. performed a retrospective epidemiological study that included over 27,000 Achilles tendon ruptures between 2001 to 2012. They found that the incidence of Achilles tendon rupture increased during this time – 17% increase in men and 22% increase in women. The actual incidence rates in 2012 were 55.2 (per 100,000 person-years) in men and 14.7 in women. For those not up with epidemiological statistics (not top priority for most clinicians), person-years is just number in population x years.
www.ncbi.nlm.nih.gov/pubmed/25081311
Kragsnaes et al. investigate the presence of immune cells in biopsies from Achilles tendinopathy and normal Achilles tendons. Macrophages and endothelial cells were greater in number in tendinopathy samples. They did not investigate cytokine release from these cells, so their role is not known. No cell type was associated with outcome at 4 years – clearly lots of confounders eg treatment, presentation, etc. Interesting finding was that biopsy induced a painful tendinopathy for 6 months in 6 of the controls (6/15=40%), but none of the tendinopathy group – so normal tendon matrix does not like being interfered with. Not consistent with low patellar tendinopathy rates reported post patellar tendon graft for ACL reconstruction.