I have have experienced physio Carly Johnson joining me in clinic over the last few weeks on her MSc placement from La Trobe Uni, Melbourne, Australia. Has made me realise how many interesting/atypical tendons I see, so we decided to blog about some of the interesting Achilles. I see about 5-10 new Achilles per week, >300 per year. I estimate 60% to be ‘boring old’ midportion or insertional tendon issues, but some are more interesting.
This blog highlights signs and symptoms of common differential diagnoses in Achilles, and how ultrasound imaging can help. I ultrasound image every single Achilles that comes through, and it has taught me lots about how pathology and symptoms interact. Ultrasound can never MAKE a diagnosis, but is excellent for CONFIRMING many conditions that present similarly to Achilles tendinopathy.
Often I see Achilles injuries that have failed treatment, and incorrect diagnosis explains a considerable number of these, so it’s important to get the right diagnosis.
Obviously there are lots of other diagnoses that have not made it into the blog, such as as sural nerve irritation, apophysitis, distal soleus muscle-tendon injury, fascia crura tears, somatic or radicular referral from lumbar spine, etc.
MIDPORTION TENDINOPATHY
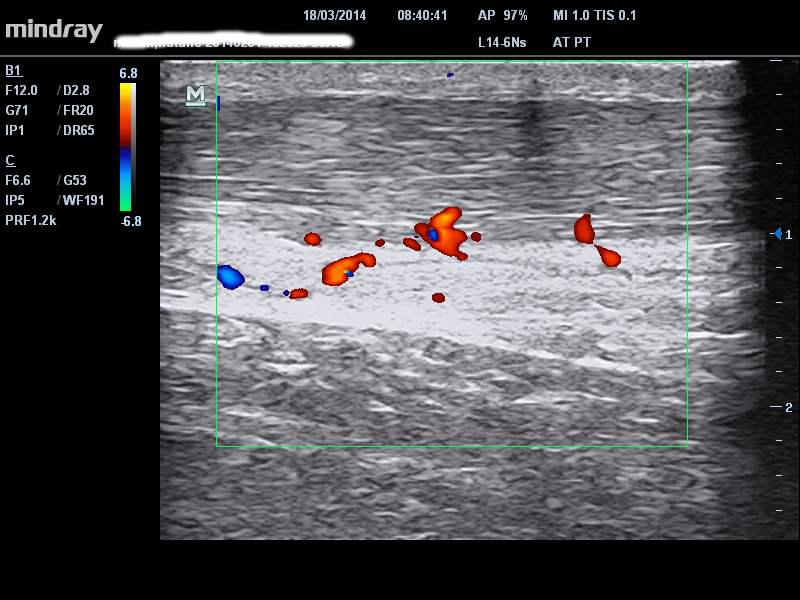
The typical symptoms of this condition include localised Achilles tendon pain that ‘warms up’ with activity. The pain is usually worse in the morning but improves after 5-10min. There is usually a history of overload of stretch shortening cycle activity like walking or running. A useful test is palpation tenderness in a stretched position verses a relaxed position (London Hospital Test). If the tendon is more painful in a relaxed position it is more likely tendon pain than pain from the surrounding tissues ie. fat pad, bursa. Imaging does not really help to confirm a diagnosis, but can be useful in identifying the extent of pathology – our patient below had diffuse minor ‘degenerative’ changes with Doppler signal, but presented with midportion pain. You would still be careful with end range loading in this case even though her symptoms are midportion, based on the finding of some low midportion/near insertion pathology.
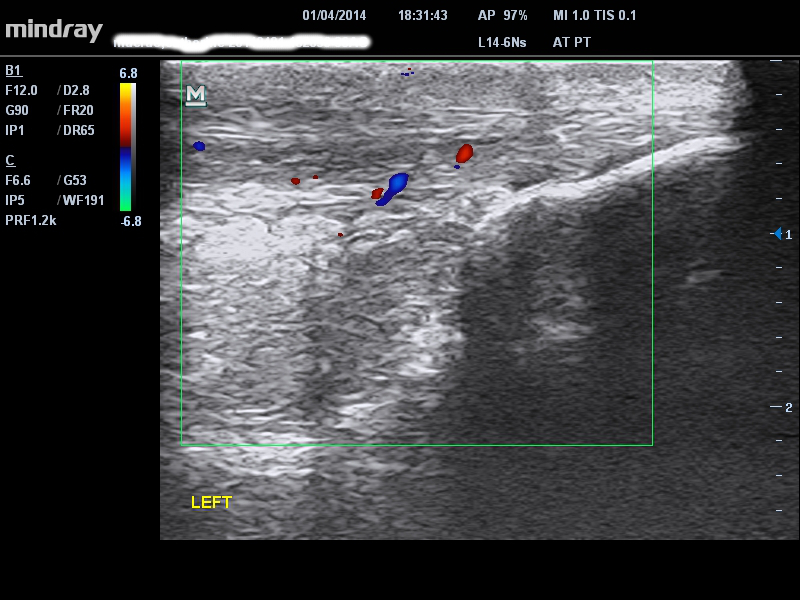 Figure 1 – diffuse midportion and low midportion (close to insertion) pathology and Doppler signal
Figure 1 – diffuse midportion and low midportion (close to insertion) pathology and Doppler signal
INSERTIONAL TENDINOPATHY
The main difference in insertional tendinopathy is the site of pain at the distal Achilles insertion either high (superior calcaneum tuberosity) or low at the distal calcaneum. There is a similar pain behaviour / morning stiffness and ‘warming up’ pattern to midportion tendinopathy. The high insertion pain needs to be differentiated from a retrocalcaneal bursa whereas the low insertional pain is often from the tendon. On ultrasound there may be an associated traction spur with the low insertion but this is not necessary symptomatic – see traction spur in figure below.
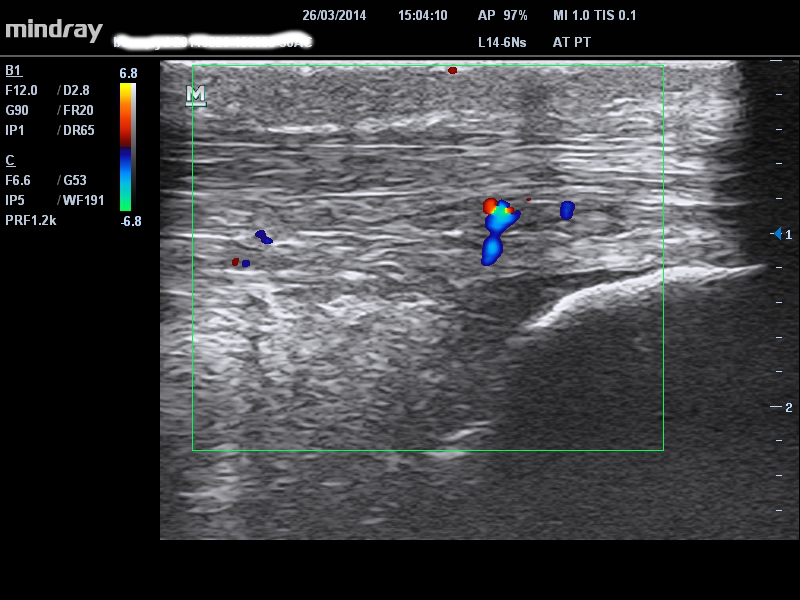 Figure 2 – high insertion tendon pathology with Doppler signal
Figure 2 – high insertion tendon pathology with Doppler signal
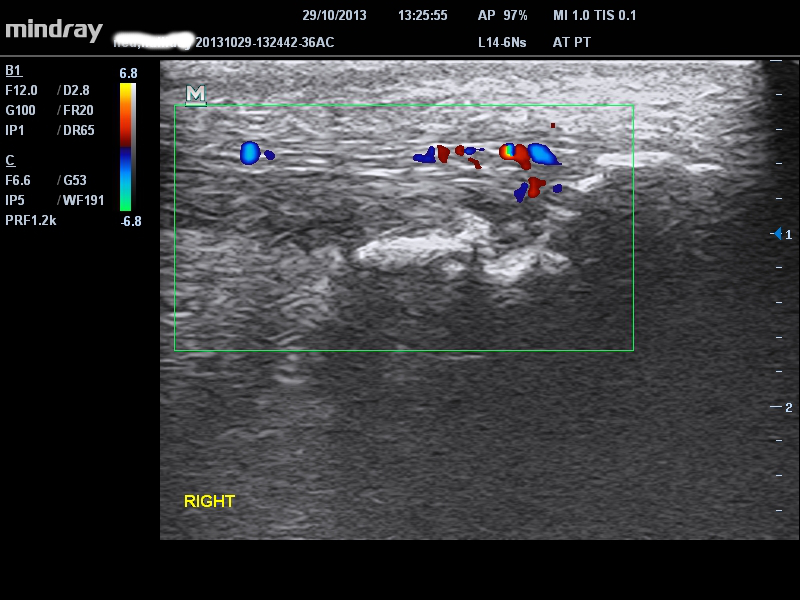 Figure 3 – low insertion tendon pathology with Doppler signal, and traction spur
Figure 3 – low insertion tendon pathology with Doppler signal, and traction spur
RETROCALCANEAL BURSA
Retrocalcaneal bursa can present with symptoms in exactly the same location as insertional tendinopathy however they may be more diffuse. One of the clues to differentiate is irritable pain and symptoms on low load activities such as heel raises or end range compression in dorsiflexion.
These symptoms may also occur in insertional tendinopathy, if it is reactive or irritable this is where ultrasound is very helpful. Differential palpation of the two tissues can also be very helpful. If there is a lot of fluid or thickening of the bursa on imaging it very likely to be a pain generator and should be treated. Conversely, a little fluid on imaging is normal in active populations. Our patient in the image below had insertional Achilles and bursa pathology and typical bursa symptoms including pain with low load activities and stretching. So treating the bursa is a priority over and above the tendon. This lady had been misdiagnosed and treated as a tendon injury and the bursa was the limiting factor.
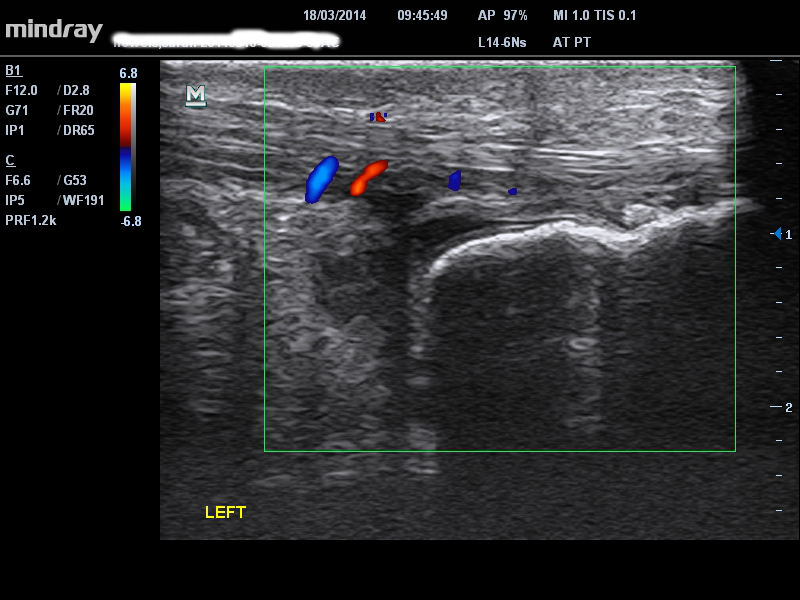 Figure 4 – high insertion tendon pathology with retrocalcaneal bursa fluid
Figure 4 – high insertion tendon pathology with retrocalcaneal bursa fluid
PARATENON
Paratenon inflammation often presents with a reactive or irritable pain that flares for days after activity and can also be painful with low load activities such as calf raises. Our patient in the image below reported pain that flared for three days after a bike ride – definitely not a high tendon lad/stretch shorten cycle activity, so an inflammatory/compressive pathology is suspected. You can see huge lateral paratenon fluid collection in the image. On assessment the London Hospital test was negative; pain was unchanged with tendon palpation in a relaxed and stretched position. Often the patient will localise to the medial or lateral side of the Achilles which is again not typical of midportion tendinopathy. When localised to the medial side there needs to be some suspicion of plantaris (see below). Ultrasound imaging is excellent for imaging plantaris tendon abnormality vs paratenon fluid vs midportion Achilles – but of course needs to be married with clinical symptoms.
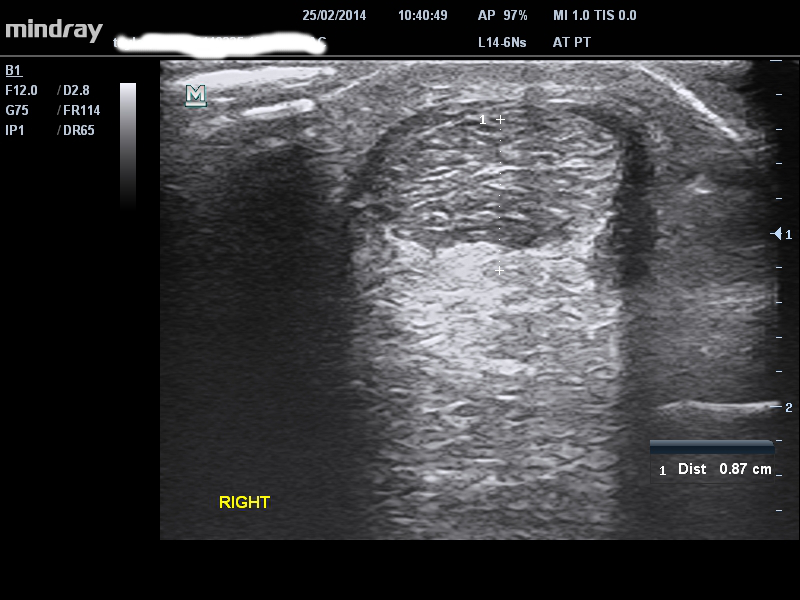 Figure 5 – huge fluid collection around lateral paratenon
Figure 5 – huge fluid collection around lateral paratenon
PLANTARIS TENDON
Can manifest as pain in the plantaris tendon, or irritation/compression of the medial Achilles tendon from the plantaris tendon. Plantaris tendon pain is not common – see example of insertional plantaris pathology in one of my patients (Figure 6) – he pointed to a very specific site of medial Achilles insertion pain – we injected with high volume saline and it never came back, despite 2 years of further track 400m competition. More common plantaris issues involve compression of the Achilles. Can be typical Achilles symptoms but more likely medially localised pain and medially localised Achilles pathology. Symptoms can come on in end range dorsiflexion from compression of the tendon. May be associated with increased foot pronation in function.
 Figure 6 – hypoechoic and thickened plantaris tendon seen medial to the Achilles at the superior calcaneum
Figure 6 – hypoechoic and thickened plantaris tendon seen medial to the Achilles at the superior calcaneum
TRUE PARTIAL TEAR
Need to have the key diagnostic signs for a partial tear – 1) definite incident that they can remember (and describe in detail, down to the minute!); 2) acute pain/definite change in pain following the incident; 3) acute and major loss of strength, related to pain inhibition. i.e. this is a major change in pain and function that you WILL be able to pick a mile away from a tendinopathy. Ultrasound often shows what is sometimes referred to as delamination of the fat pad and tendon, with a definite hypo- or an-echoic region – ie a black hole, that is continuous with the periphery of the tendon.
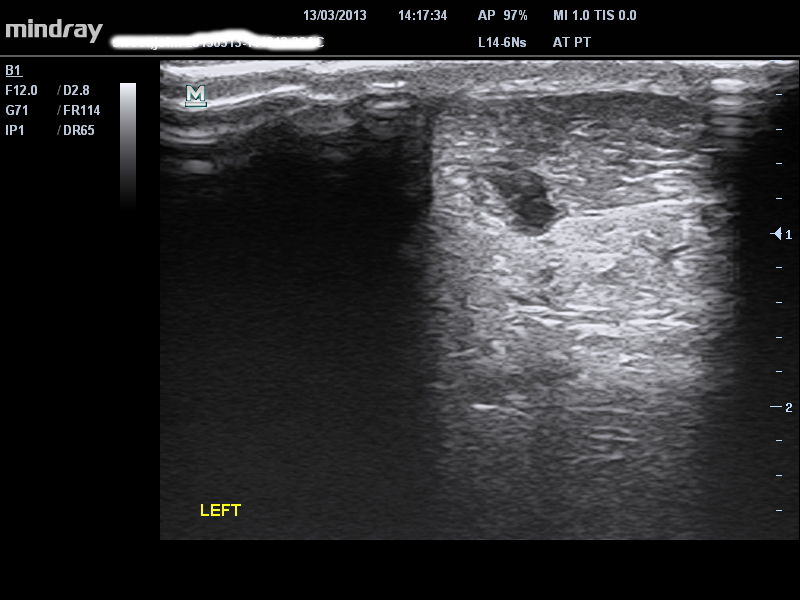 Figure 8 – very localised hypo/anechoic region in a patient presenting with signs/symptoms of a tear
Figure 8 – very localised hypo/anechoic region in a patient presenting with signs/symptoms of a tear
ACCESSORY SOLEUS
Accessory soleus is very rare. I have see 4-5 in ten years. Usually presents with pain around the Achilles but on closer inspection deep to the Achilles tendon. There is an obvious muscle bulk very low deep to the Achilles on both the medial and lateral sides and often tender on palpation. The main differential diagnostic sign is that pain gets worse with activity and does not warm up with activity, similar to compartment syndrome. Ultrasound is very useful in confirming that there is a low lying soleus (or accessory) soleus. Our patient in the image below had a distal soleus to superior calcaneum length of 1.6cm whereas most people have at least 3-4cm. This guy had been misdiagnosed and given 2 PRP injections into a normal tendon !! A true accessory soleus reportedly inserts into the calcaneum – I have never seen this. So maybe the more common variant that I have described here should be called a ‘low soleus’.
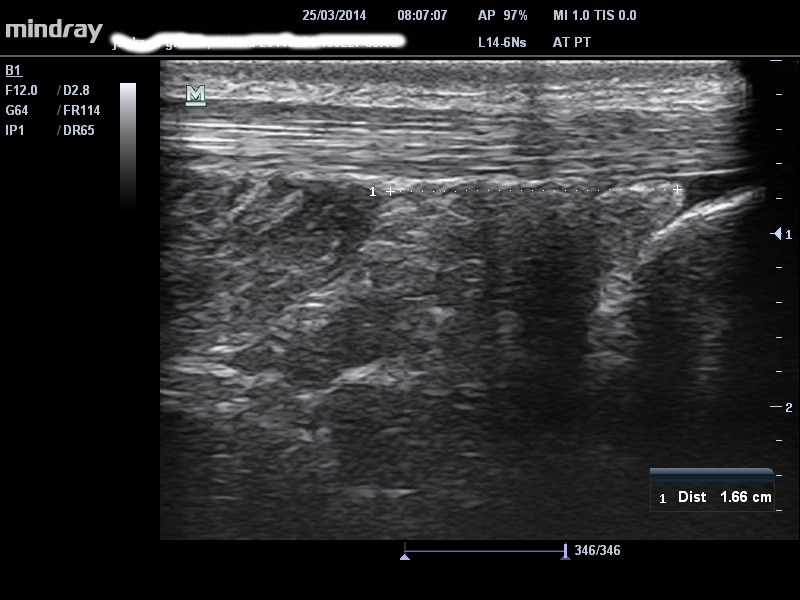 Figure 9 – 1.66cm distance between distal soleus and proximal calcaneum in a patient with symptomatic accessory soleus
Figure 9 – 1.66cm distance between distal soleus and proximal calcaneum in a patient with symptomatic accessory soleus
FAT PAD
The fat pad can give symptoms isolation, commonly from compression in dorsiflexion, often when there is an associated but asymptomatic thickened tendon, accessory/low soleus or abnormal plantaris tendon. It is usually the fat pad around the proximal/midportion of the Achilles that is affected, rather than more distally. Pain can be diffuse medial and lateral or medial only. The diagnosis is always clinical and based on differential palpation of the fat pad and tendon – simple but often missed! Also, the fat pad may warm up less well and be more irritable. Ultrasound sometimes gives Doppler signal in the fat pad mainly, as seen below, but this is bot consistent.
Figure 10 – Doppler signal in fat pad but predominantly deeper fatty tissue in patient with fat pad symptoms
Hope you enjoyed
All the best
Peter Malliaras & Carly Johnson